Is This the Time to Amp Up Your Care Management System? YES
No matter how good your care management software platform is, there are a number of factors that may be contributing to suboptimal performance, especially our rapidly-evolving environment.
External factors that drive a need to reexamine the implementation of your system include:
- The expansion of value-based care causing a sharpened focus on population health management
- The evolving concept of whole-person care and the need for coordinated care activities
- The enhanced collaboration between payers and providers – partially driven by value-based arrangements
- The pace of new regulatory requirements (e.g., same-day prior authorizations)
Internal factors that may be contributing to suboptimal operational performance, especially if your system has been in place for a long time include:
- How well the inherent capabilities of the software itself are used
- How the software was implemented, including configuration, workflow design, etc.
- How well the system is maintained and managed (keeping up to date with software releases, keeping in-house expertise up to date, participating in the vendor’s user community)
- How well the system is integrated with other systems and with the outside world (e.g., HIEs for the exchange of ADT and clinical information)
- How efficiently the system is used, including the proficiency of staff, standardization of processes, and how work and workloads are managed
- How effective the operation overall are – including quality and other performance measures
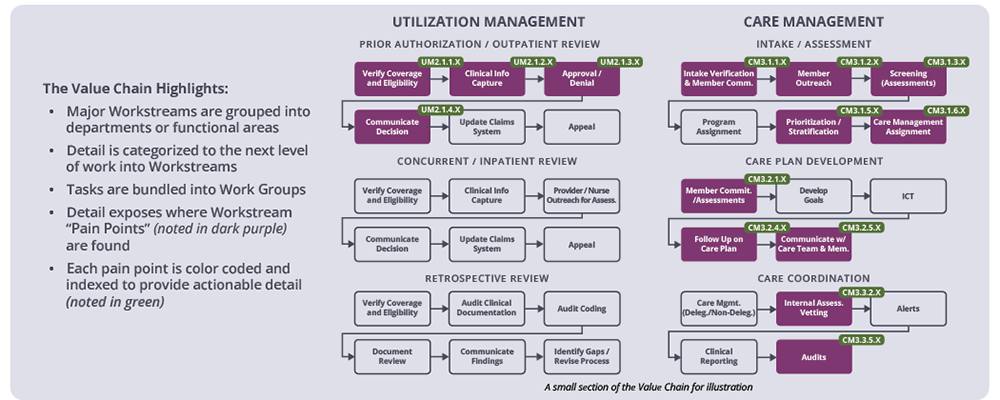
Ironwood Health has developed a framework for the assessment and optimization of clinical operations performance that is based upon the concept of a Value Chain. The Value Chain is a visual representation of large groupings of organizational work. It identifies operational “pains points” that contribute to workflow inefficiencies. The Value Chain then acts to promote an organization-wide understanding and agreement of challenges, and is used to identify opportunities improvement and optimization.
The overarching goals for such improvement will frequently involve providing access to a common, longitudinal view of the patient/member that assures everyone is on the same page and has a shared understanding of what’s happening, and what may be next. The goal of breaking down operational silos in care and eliminating redundant or manual work (e.g., overlapping communications to the consumer and records kept outside the system) can reduce turnaround times, improve responsiveness, and eliminate friction.
And finally, improved care management operations can lead to better patient outcomes and significant improvements in the healthcare consumer experience. When healthcare operations can effectively coordinate care, ensure adherence to treatment plans, and monitor patients’ progress, the likelihood of positive health outcomes increases. This level of management translates to healthier, happier patients who recover more quickly, experience fewer complications, and require fewer costly interventions (such as hospital readmissions).
By applying sustained focus, healthcare organizations can improve care management operations, enhance the healthcare experience and provide more effective, patient-centered care.